
The Covid pandemic has been devastating for the world, with 6.8 million deaths. In the UK, 206,000 people have died from Covid-related causes. As pandemics go, it’s by no means the worst. The 1918 flu pandemic killed 20-50 million people, and the Black Death, caused by the bubonic plague bacterium, killed around 75-200 million people, or around half the world’s population. What was different about Covid was the development of vaccines, in particular RNA vaccines. And with that development of RNA vaccines came a new possibility: a cure for cancer. In this blog post, I’ll try to explain what RNA vaccines are, how they work, and why they could be the key to creating bespoke treatments for cancer.
Cancer remains the world’s second biggest cause of human death, behind cardiovascular disease. Over ten million people a year die from cancer, worldwide. But a universal cure for cancer has remained elusive. That’s largely because cancer tumours are unique to the individual, and are very similar in their physiology to the rest of our bodies. Treatments such as chemotherapy work on the principle that because cancer cells are more active and grow faster than other cells, they will be more affected by toxins. Chemotherapy agents are sophisticated, but are basically poisons that can cause lasting damage to healthy cells, too.
 With the development of RNA vaccines, a new potential way to treat cancer has arrived. This involves effectively immunising the body against its own cancer by identifying proteins in the cancer that aren’t present in healthy cells, and priming the immune system to attack them. To understand how that works, it’s first necessary to understand what RNA is and how it works. And to understand that, we need to understand the basics of how the genetic code carried on DNA is translated into a life form. As you might know that bit already, I’ve explained it in another post called What Watson and Crick Were On About. But to condense it into a rather undersized nutshell, Ribose Nucleic Acid (RNA) is a chemical in our cells that helps translate the genetic code within our DNA into what we are. It transcribes the DNA code from the DNA in the cell nucleus to a structure in the cell cytoplasm called a ribosome, where it programmes the assembly of amino acids into proteins. It’s a messenger, so this form is known as m-RNA.
With the development of RNA vaccines, a new potential way to treat cancer has arrived. This involves effectively immunising the body against its own cancer by identifying proteins in the cancer that aren’t present in healthy cells, and priming the immune system to attack them. To understand how that works, it’s first necessary to understand what RNA is and how it works. And to understand that, we need to understand the basics of how the genetic code carried on DNA is translated into a life form. As you might know that bit already, I’ve explained it in another post called What Watson and Crick Were On About. But to condense it into a rather undersized nutshell, Ribose Nucleic Acid (RNA) is a chemical in our cells that helps translate the genetic code within our DNA into what we are. It transcribes the DNA code from the DNA in the cell nucleus to a structure in the cell cytoplasm called a ribosome, where it programmes the assembly of amino acids into proteins. It’s a messenger, so this form is known as m-RNA.
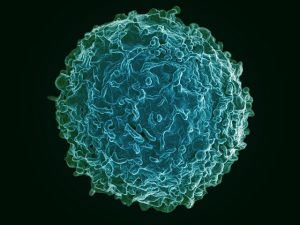
So what has all this got to do with new cancer drugs? Let’s go back to our Covid vaccines. Traditionally, since Edward Jenner first infected an unfortunate child with cowpox to see if it would make him immune from the similar but much more serious smallpox, vaccinations had worked in the same way. Bits of protein, usually derived from dead or attenuated viruses, were injected into the patient to stimulate an immune response. The host body, thinking it was under attack from the virus, would produce lots of antibodies to attack these proteins, meaning that if the live virus gets into the body, there are already lots of ready-made antibodies there, making it much easier to fight off the virus. These antibodies are made in a type of white blood cell called b-lymphocytes. They work in several ways, but commonly stick to the proteins (antigens) on bacteria and viruses, clumping them together and preventing them getting inside cells and multiplying. These neutralised clumps can then be gobbled up by another type of white blood cell called a phagocyte. This immune response is also carried out by the exotically-named ‘killer t-cells’ … more about those later.

The Oxford AstraZeneca vaccine, the first to be licenced for widespread use in the Covid pandemic, was one of these traditional vaccines. Such vaccines are expensive and time-consuming to produce, normally taking around 20 years from initial development to full implementation. So it was a remarkable achievement by the largely female team, led by Sarah Gilbert, to develop a vaccine in less than a year. However, after saving possibly millions of lives, the vaccine was rendered obsolete by the development of new RNA vaccines. These vaccines (for Covid, the Pfizer and Moderna vaccines), work in a different way. They involve injecting synthetic m-RNA molecules into the patient, which get into the patient’s cells, attach to the ribosomes, and programme the production of viral antigens. Once released from the cell into the blood, this viral protein produced by the patient’s own cells triggers an immune response in the same way as with a conventional vaccine. Before Covid, these vaccines had been used in limited ways. They have a big advantage in that they are much quicker and simpler to develop than a conventional vaccine. But there are disadvantages. The m-RNA is unstable, and it’s difficult to get it into the patient’s cells. It’s also recognised as foreign RNA by the body’s immune system, and destroyed before it gets into a cell. But during the Covid pandemic, research on RNA vaccines was massively accelerated too, packing work that would have taken 20 years or more into a few months. One of the ways developed to protect the m-RNA so the body’s immune system doesn’t recognise it is lipid (fat) encapsulation, which is a means by which bacteria can evade attack from the immune system, or from food preservation techniques, that I worked on way back in the 1970s.
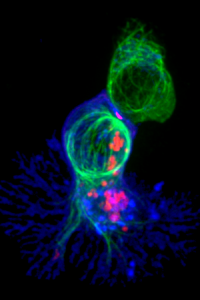
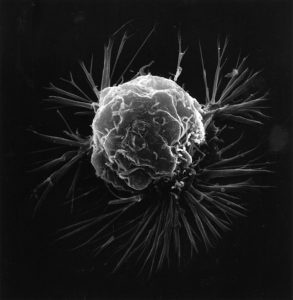
So far so good. But what’s the impact of all this on curing cancer? Cancer cells are, like viruses and bacteria, foreign cells in our bodies. But they’re not all that foreign – they have after all mutated from our own cells. Nevertheless, there are differences, and our immune system can recognise them. Cancer cells appear in our bodies all the time, and are quickly dealt with by our immune system, usually by killer t-cells that recognise infected or foreign cells and destroy them. This is more difficult with a cancer than with an infection, partly because the cancer cell is derived from our own cells, and partly because there are only a few of them, so they don’t trigger much of a response. But sometimes, a cancer cell might appear that reproduces a bit too fast for our t-cells to cope with. In that case, our immune system might keep it in check for years without actually destroying it, or it might start to overwhelm our immune system. As the cancer grows and the cells replicate, they start to develop new techniques to evade our immune response. They can change the antigens on the surface of their cells to confuse our immune response (like the way a new strain of Covid reduces the effectiveness of vaccines and can evade the body’s immune response). Or they can create a ‘hostile environment’, releasing chemicals that stop t-cells from working.
Conventional vaccines are not much use here. Every tumour is different, and specific to the patient. But because RNA vaccines are ‘bespoke’, they can be tailored to produce the very specific proteins in an individual patient’s cancer. Clinicians remove some cancer cells and isolate proteins not found in the patient’s healthy cells. They then make an RNA vaccine that codes for the production of just that specific protein. When this bespoke RNA gets into the patient’s healthy cells, it uses their own ribosomes to make these cancer cell proteins. These proteins, on their own, are entirely harmless. But they can then trigger a whole-body programming of killer t-cells to destroy cancer cells that contain this foreign protein, leaving alone the healthy cells that don’t contain it. RNA vaccines can even programme for the production of special proteins that neutralise the hostile environment created by tumours, allowing t-cells to do their job more effectively. And there it is: potentially, a cure for cancer.
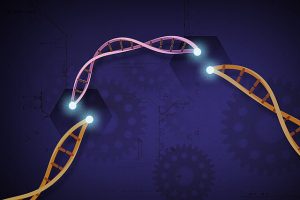
One question that might have occurred to you by now, if you’ve been paying attention, is: so why inject people with RNA to make specific proteins? Why not go one step further and insert new DNA into their cells that will make the RNA in situ? Firstly, it’s much harder to get DNA into a cell nucleus. And once inserted into the genome, the DNA will keep on churning out the programmed RNA for the rest of your life. And there are ethical questions about modifying someone’s genes. Having said that, it is possible. There’s a technique with the catchy name of Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR), cadged from bacterial viral defence systems (yes, even bacteria get infected by viruses), which does precisely that. It pre-dates Covid by ten years or so, and has been used in trials to treat sickle cell anaemia, by snipping out the gene that programmes for faulty red blood cells and replacing it with a gene that produces good ones. It’s a ‘gene editing’ process, and could be used on embryos containing faulty genes. That’s an ethical minefield of course – what’s your definition of ‘faulty’? Sickle cell? Genetically derived cancers? Down’s Syndrome? Cystic Fibrosis? Ginger hair? Brown eyes? Dark skin? It’s what eugenicists could only have dreamed of … another blog post, perhaps.
At the moment, all these techniques are experimental, although are now being tested in clinical trials. But we have Covid to thank for the fast-tracking of RNA vaccine research, and the development of ways by which bespoke RNA can be produced, and protected so it can be delivered into cells. Without the Covid pandemic and the rush to get a mass Covid vaccine, the development of RNA vaccines for cancer would be not just a few years away, but decades away. Now, the prospect of a genuine cure for cancer, through bespoke, personal vaccines tailored for each individual cancer in each individual patient, is a real prospect. It is though worth bearing in mind that all this was achieved because of the effect of Covid on the world economy. When the wealth of those with the power is threatened, mountains can be moved. Imagine what we could achieve if society was run for the benefit of us all, rather than responding only when there’s a threat to the interests of capital.
